Reproducible freezing and thawing is critical for successful cell therapies. Cytiva’s G. John Morris explains why.
Originally published in the Medicine Maker – www.themedicinemaker.com
The potential of cell therapies has been recognized for some time, but commercialization is a relatively recent endeavor. Cryopreservation is a crucial part of the manufacturing process, because it allows cell therapies to be efficiently stored and transported; however, it is only beneficial if cell viability is maintained. Here, we speak with Asymptote (now part of Cytiva) CEO John Morris, who has been freezing cells for over 40 years, to delve into the good, the bad, and the icy aspects of cryopreservation.
How did you become involved with Asymptote and GE?
Back in the 1970s, my PhD focused on the freezing of T and B lymphocytes, which was widely ignored at the time. I was fascinated by the field and I worked for various research councils on freezing-based issues, such as how organisms grow in the Antarctic or on high-altitude mountains. Soon after, I dabbled in the academic world before joining Asymptote in 1989, where I worked on a range of freezing/solidification challenges across a wide range of industries, from food products such as ice cream, to freeze drying of pharmaceuticals and oil and gas industry projects. Early in 2017, after identifying the work we were doing, Cytiva acquired Asymptote to fill a critical gap in Cytiva’s end-to-end ecosystem of products and services for cell therapy production, and form an important piece of its cell therapy portfolio.
How have cell therapies changed the approach to cryopreservation?
Cryopreservation was developed in the 1950s, mainly for shipping livestock sperm worldwide. In time, it was applied to other cells, such as human sperm, embryos, and blood cells. Around 10 years ago, regenerative medicine became a reality and cells were being classified as medicinal products, which led to a need for better control over the freezing and thawing process. For example, when freezing many different samples, you have to ensure that each sample has the same activity once thawed. Each sample also has to be free from contamination, and you have to be able to track everything to ensure the patient gets the right cells.
We spoke with Innovate UK, a funding body, about the changes taking place in the field. They identified clinical delivery of cells in regenerative medicine as a gap in the industry. Cells were being grown and created for therapeutics, but people were not putting much thought into the post-manufacturing steps of getting cells to the patient. To help fill that role, Innovate UK awarded us several grants to develop equipment and consumables that help deliver cryopreserved cells for clinical use. We also teamed up with the UK’s Cell and Gene Therapy Catapult to work on the final stage of the chain – an instrument to thaw the cells for clinical application.
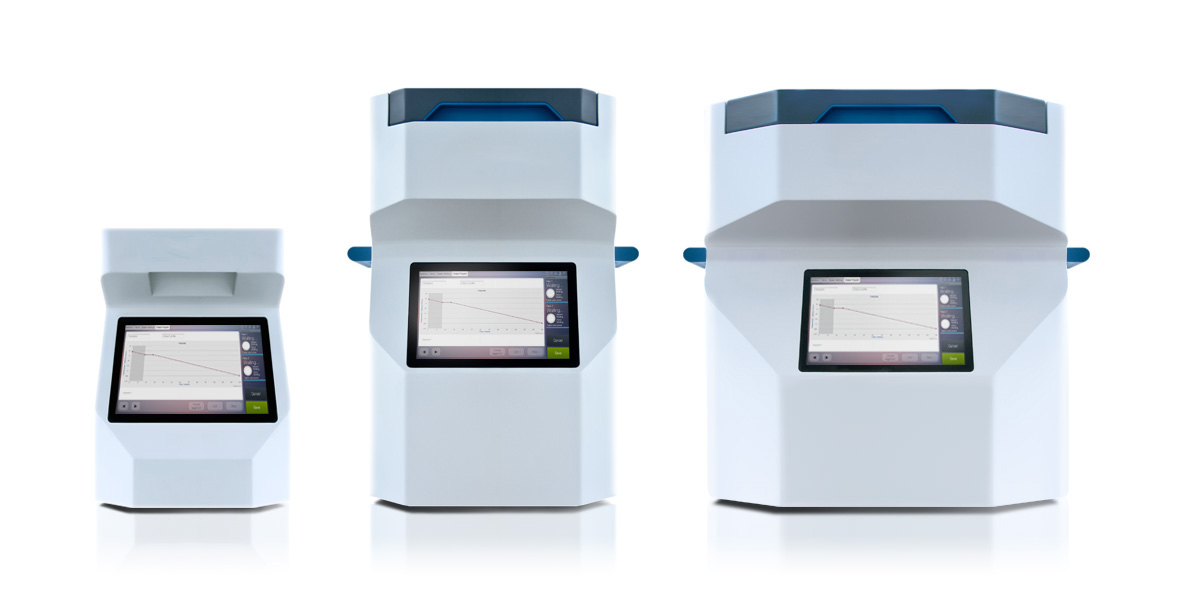
Cytiva’s VIA Freeze range of liquid nitrogen-free, controlled-rate freezers.
How is the industry reacting to commercialization pressures and the need for cryopreservation?
We have been working with leaders in the cell therapy field for around 10 years, and it has been interesting to watch the field develop. Right now [in 2017], it is exciting to see immunotherapies close to reaching healthcare systems, with companies like Novartis and Bluebird Bio looking to get immunotherapies approved in the US. However, now that the research is coming to fruition, the industry is suddenly realizing that the cryochain – cryogenic cold chain – will be critical to its success.
One of the main reasons for cryopreservation is quality control. For example, when producing immunotherapies, you need to test that the T cells you have grown are the correct type, that they do not contain bacteria, and that they are fit for use. This takes several days – and cryoprocessing helps buy back time. It is also important to consider the patient. Patients, by definition, are often very ill, and complications might mean that they are unable to receive immunotherapy on the planned day. Frozen therapies can easily be stored, allowing for more flexibility in terms of when they are administered. Cryopreservation also has benefits from a financial perspective – shipping fresh cells is far more expensive than shipping a frozen product.
What cryopreservation pain points are cell therapy manufacturers likely to face?
Companies can get so caught up in the intricacies of the biology that the cryopreservation and shipping aspects become an afterthought. Freezing a few cells in the lab is easy for research applications, but freezing cells that will be injected into patients as therapeutic drugs is more challenging – and often underestimated. Now, many big companies are realizing that they have to get the cryogenic cold chain correct, and are hiring PhD cryobiologists. Some think that refrigeration at 4°C is a good short-term alternative, but it is actually significantly more expensive to refrigerate cells and maintain a regular cold chain than it is to cryopreserve cells and ship them at cryogenic temperatures. Cell therapies are already expensive to produce, so I do not believe that refrigeration is a sustainable solution.
Retaining cell viability and function on thawing is one of the biggest challenges, which means that you need to plan your cryopreservation strategy at an early stage. In other sectors of cryopreservation, peak viability is not necessarily crucial. For example, there are around 200 million calves born every year following artificial insemination with cryopreserved sperm. Whether 100 percent or 10 percent of the sperm are viable is irrelevant so long as one of them can fertilize the ovum. With cell therapies, however, low viability is not an option; it essentially means that the patient gets a lower ‘dose’ of therapy, which can prevent treatment from working effectively.
There are many factors that come together to help maintain high cell viability, including experience and the equipment used. Asymptote (now part of Cytiva) has been working with cells and cryopreservation for years, so we understand the ins and outs of the process. When somebody approaches us with a clinical treatment that they want to develop, we look at how best to tailor the cryopreservation process to their particular cells. Controlling the temperature of ice formation during cooling or using the right cooling rate, for example, can double or triple viability compared with other techniques. It is all about knowledge and experience – understanding and controlling what works in terms of cooling, storing, and thawing.
How has cryopreservation equipment evolved over the years?
Until about 10 years ago, equipment was based on liquid nitrogen, which worked well for many types of cells. When we are effectively dealing with medicines, however, it is not the right solution – liquid nitrogen is often contaminated with particles and biologically active bacteria. Because of this – and the fact that liquid nitrogen is quite hazardous to operate with – we turned to Stirling cryocoolers. Not only do they provide more control over the processes, they are also safer and simpler to use than liquid nitrogen. A huge amount of engineering and refinement has gone into optimizing these cryocoolers (they were previously used by NASA and the European Space Agency for use on the space station), and our company has pioneered their application in cryopreservation.
At the moment, scaling is one of the main limitations with equipment. We are currently performing batch freezes of small samples at a time, which is adequate for today’s needs. But in the not-too-distant future I believe there will be a surge in demand, and equipment will need to keep up. For example, continuous processing of large batches will be required as allogeneic therapies come to market. I also expect equipment to advance in terms of tracking capabilities. We can already track cells to an extent but, in time, it should be possible to obtain a complete history of the cells from creation to patient. This digital backbone will allow us to further control the temperature and condition of the samples in real time. We might even get to the point where patients can watch their therapeutics move through the supply chain towards them.