The Center for Advanced Therapeutic Cell Technologies (CATCT) helps companies and researchers to scale faster.
Nicole Gularte was 26 years old and straight out of graduate school when she was diagnosed with acute lymphoblastic leukemia, also known as ALL, in 2010. This type of fast-moving blood cancer causes the bone marrow to produce too many immature white blood cells, called lymphocytes, which can spread the disease to other parts of the body. If left untreated, it can turn deadly within months.
Determined to keep fighting, Gularte decided to try a different tactic: enroll in an experimental treatment known as CAR-T therapy, which uses her own immune cells that have been reengineered to find and kill the cancer.
For CAR-T, doctors extract a patient’s T cells and send them to a lab where they’re carefully reengineered and multiplied so they can sniff out the cancer cells and mark them for destruction. Then the manipulated cells are shipped back to the patient’s treatment location, where they’re injected back into the patient’s bloodstream so they can do their work. The therapy, developed by doctors at Children’s Hospital of Philadelphia, gained fame after it saved a young girl named Emily Whitehead in 2012. With guidance and encouragement from Emily, her family and the Emily Whitehead Foundation, Gularte received her own modified cells a year ago, and she’s now cancer-free. “I have officially survived acute lymphoblastic leukemia eight times,” she wrote on her blog.
The good news is that stories like Whitehead’s and Gularte’s could soon become more common. In August, the U.S. Food Drug Administration approved the first cell therapy in the United States for the treatment of pediatric and young-adult patients with a form of ALL. “We’re entering a new frontier in medical innovation with the ability to reprogram a patient’s own cells to attack a deadly cancer,” said FDA commissioner Scott Gottlieb.
But cell therapy is a complex process that involves more than manufacturing a pill. It requires a setup that resembles a biotech factory. “Cell therapy has the potential to cure everything from cancer to diabetes,” says Phil Vanek, general manager for cell therapy growth strategy at Cytiva. “But we need to make it affordable and scalable.”
Vanek’s business and others are racing to make that happen and deliver on cell therapy’s promise. He says that says that hundreds of patients have already benefited from CAR-T in clinical trials that have reported 80 percent success rates. Some 300,000 people could be receiving the treatment by 2024. A report by Roots Analysis estimates the T-cell therapy market, which includes CAR-T therapy, could read $30 billion by 2030.
Crucial to that race is a new cell therapy research and process-development facility called the Center for Advanced Therapeutic Cell Technologies (CATCT), which officially opened in Toronto in September. It’s designed to help pharma companies, university researchers and technology companies like Cytiva to scale faster. “Right now, the technologies and production methodologies can support a few hundreds to a few thousands of patients, but it’s still a brute-force approach,” Vanek says. “The manufacturing process is not easy, it’s not automated, and it requires quite a bit of hands-on labor. It has to change to support the broader patient population, and it will.”
Led by Canada’s Centre for Commercialization of Regenerative Medicine, a leader in developing and commercializing cell and gene therapies and regenerative medicine technologies, the new Toronto center already employs more than 30 biologists, virologists, and biomedical and other engineers, including some from Cytiva.
Cytiva helped fund and equip the lab, and the researchers are using bioreactors to grow engineered cells and identify the optimum growing conditions for different cell types, laser-powered flow cytometers that can study the properties of individual cells, and even robots running production automation experiments.
One purpose of CATCT is to develop new processes that will enable pharma companies to offer cell therapy to millions of patients. Despite success stories like Whitehead’s and Gularte’s, the vast majority of new cancer patients still start with standard treatments like chemotherapy, and the FDA approved the first CAR-T treatment only for patients with “refractory,” or resistant, cancers, or those in second or later relapses. But “if these therapies move to a first-line treatment, then the number of patients will go up dramatically into the hundreds of thousands, if not more,” says Vanek.
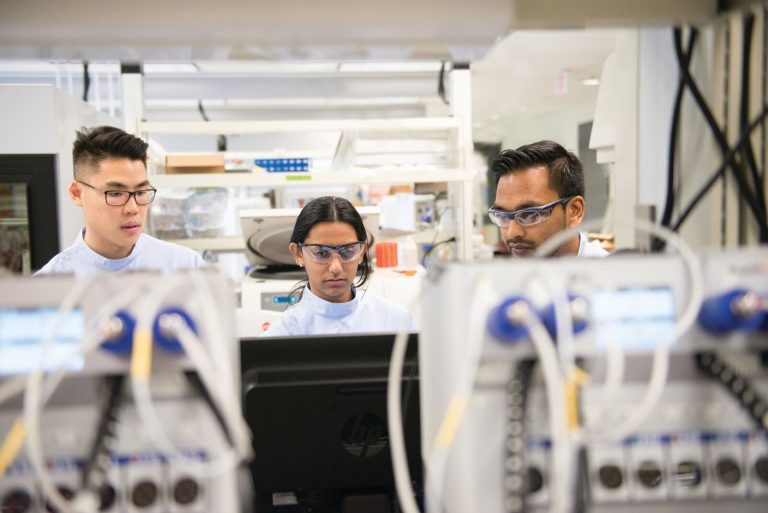
Image credit: CCRM
Vanek says that CATCT will allow technology companies like Cytiva to learn about new therapies in the pipeline. “This was our blind spot in the past,” he says. “You really need to walk in the shoes of our customers to understand where their pain points and challenges are.” He also said that partners working at the center — big companies as well as universities and startups — will have access to a “fee for service” process-development capability. “This makes the group not only self-sustaining by taking on client work,” he says. “It will also give us access to more customers who will come to us with their toughest challenges, and that’s where the learning happens.”