One way to speed up the manufacturing process is FlexFactory for cell therapy.
In October, scientists in Boston revealed they’d used genetically modified cells to cure 15 boys of a nerve disease that until now has been nearly 100 percent fatal. During a clinical trial, which lasted two years, doctors used experimental gene therapy to treat the boys with their own engineered cells. When the results came in, 15 of the 17 boys had no remaining disabilities.
Cell therapy is a new way to treat serious diseases like cancer by extracting living cells from a donor or a patient, changing them so they can recognize and attack diseased cells or deliver treatment, and returning them to the patient’s body. But manufacturing the cells is a costly and time-consuming endeavor. A single dose can cost hundreds of thousands of dollars to make.
That’s because in the more than 900 ongoing regenerative medicine trials worldwide — a 19 percent jump since 2016 — researchers generally manufacture each patient’s dose of bioengineered cells by hand. The individualized nature of cell therapy makes it not only prohibitively pricey, but also difficult to scale into commercial production.
That hasn’t been a problem while cell therapy was still confined to research labs. But as medical science advances and regulators approve a growing numbers of modified cell therapies for general use, handcrafting doses won’t be enough. “It’s relatively easy to do 15 or 20 doses by hand, but it’s nearly impossible to efficiently make thousands,” says Cytiva's Aaron Dulgar-Tulloch, director of cell therapy research and development at the Centre for Advanced Therapeutic Cell Technologies (CATCT) in Toronto.
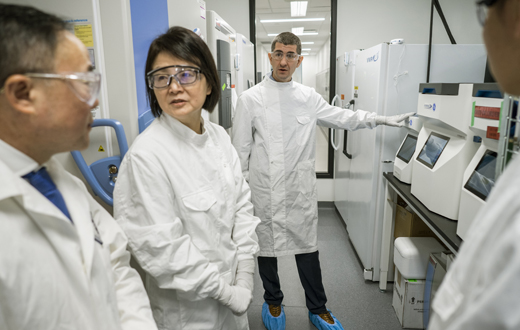
Above: Cytiva is working with the Centre for Commercialization of Regenerative Medicine (CCRM) in Toronto to commercialize cell therapy. Top: As medical science advances and increasing numbers of modified cell therapies are approved for general use, handcrafting doses will be too slow to scale. Images credit: Cytiva.
Manufacturing bioengineered cells is a delicate, multistep process that requires specific modifications to the cells at specified times over the course of hours or days. Every time a researcher works on the cells — say moving them from a sterile cabinet to a centrifuge or adding new genetic material — there’s a chance of contamination or error.
Each FlexFactory is unique and customized with the right equipment and process-development services that customers need to support individual manufacturing steps such as separating cell contents via centrifuge, freezing or thawing cells to preserve them, or harvesting the modified cells into a dose. The cells are in a sterile, closed system, and the automation leads to faster production compared with traditional small-scale manufacturing methods. “FlexFactory for cell therapy allows a company to manufacture multiple (doses) for multiple, unique patients at a faster speed,” Dulgar-Tulloch says.
The FlexFactory is also easier to install than traditional methods. It can be operational in nine months, about half the time it would require a company to make a traditional lab ready for industrial-scale cell manufacturing. CBMG’s should be up and running by the end of the year.
CBMG decided the only way to make cell therapy commercially viable was to bring down the cost. “If the price is too high and no one can afford it, cell therapy is not practical,” says Tony (Bizuo) Liu, CBMG’s chief executive officer.
